The Road to Re-Wiring: My Personal Experience of Rehabilitation
Hitting rock bottom with Functional Neurological Disorder (FND), I knew something had to change, and that ‘something’ was rehabilitation.
My situation prior to rehab was dire, to say the least.
Since, I had limited control of my movements and I was falling over 4-5 times a day even with the aid of crutches.
I also was suffering from chronic fatigue which limited my activity to 5-10 mins at a time.
By the time I was diagnosed with FND by the neurologist in November 2024, I was having extreme difficulty walking.
Deciding to go to rehab was an easy choice to make, Although I had to fight with my psychiatrist for two months before he agreed to submit the application. He was convinced my symptoms were caused solely by stress.
In this post, I will share my experiences of spending three months in a rehabilitation center to help you understand what rehab is really like and also to decide if it’s the right path for you.
Note: Its my personal experience and should not be taken as medical advice.
Prior to starting in the Rehabilitation clinic, I started repetitive Transcranial Magnetic Simulation (rTMS)
Read more on my experience of rTMS –

Pre-Rehab: Preparation & Initial Thoughts
How did I Research & Choose a Clinic?:
- Finding a Clinic: The easy part was getting recommendations from my neurologist and psychiatrist. However, it was challenging to gain acceptance into a clinic because, in France, FND is not prioritized for rehabilitation. Ultimately, I was accepted into a clinic for obesity—luckily, since I was in need of a summer body!
- Criteria considered: I focused on two primary criteria: a full-time placement and the clinic having a rehabilitation clinic. Additionally, it was a bonus if they had experience with Functional Neurological Disorder (FND) or treating patients with neurological conditions.
- My Initial thoughts: I was hopeful, knowing research shows rehabilitation is effective in about 70% of cases. Still, I worried—what if I’m in the 30% for whom the treatment doesn’t work? What would happen next?
What Practical Preparations did I make?
- Items packed: I packed the essentials everyday clothes, workout attire, towels, toiletries. I also took books to read, Sudoku puzzles, my laptop, and my guitar.
- Home life Preparation: I transitioned directly from the psychiatric hospital, where I had stayed for five months and then to the rehabilitation center.
- Admission Process: Before admission to the clinic, I provided copies of my identity documents, health card, and medical insurance card as proof of payment coverage by the insurance provider.

Life inside the Rehabilitation Clinic
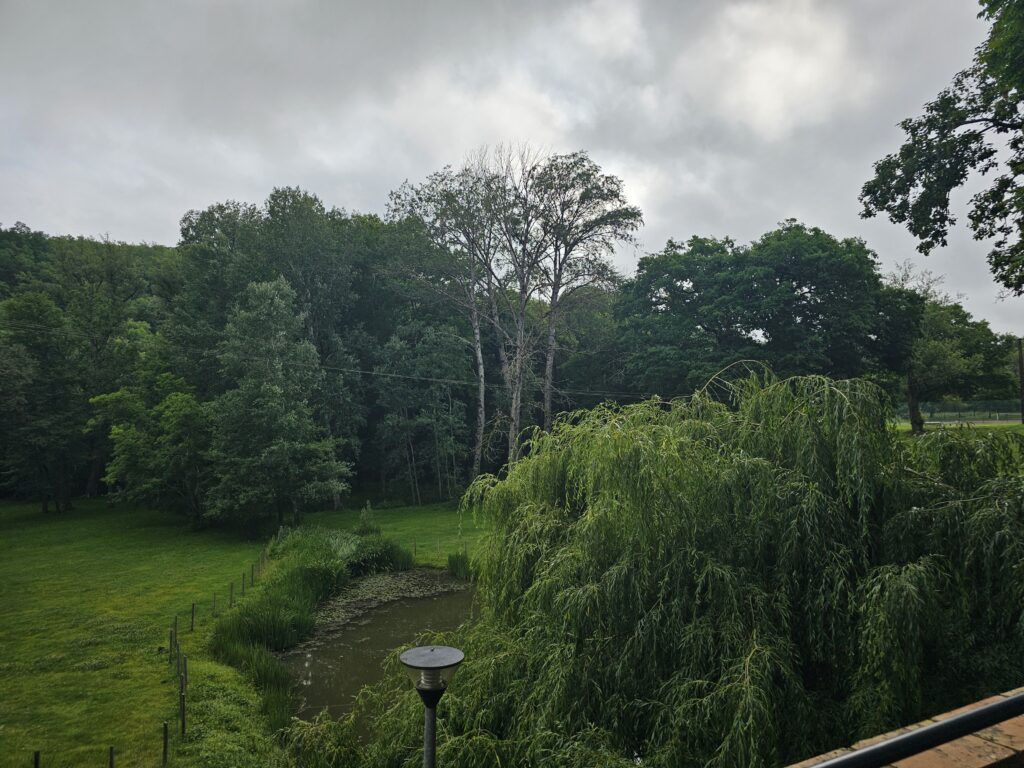
Where was my rehabilitation located?
The rehabilitation clinic was situated in the north-west of Toulouse, France in a small village called Bondigoux.
The environment was peaceful, except at night when the frogs in the pond were croaking loudly!
There were three walking routes available in the park, which ranged from 200 meters up to 1 kilometer.


What was my weekly routine?
Each day started with breakfast at 7.30am and then normally the first activity started at 9am with the physiotherapy.
Below you will see the typical weekly agenda.
- 1 session per day of Physiotherapy except the weekends
- 3 group sessions of sport
- 3 to 4 sessions on the anti-gravity treadmill
What did I do in the Physiotherapy Sessions?
They gradually increased the intensity over the three months by tailoring each session to my energy levels.
The first month focused on coordination exercises using the feet and hands, such as throwing a ball from one hand to the other, and passing the ball between both feet.
I also did a lot of work with the parallel bars, mainly focussed on walking ‘heel-to-toe’
As my energy levels improved, then the exercises became more challenging.
I had to stand on one leg on a balance mat while moving a ball around it. Additionally, I balanced on a stability ball as I threw and caught another ball.
By the third month, they had begun to introduce exercises that would strengthen my leg muscles. These exercises included squats, crab banded walks, and leg extensions.
I was also using the balance board, either with both feet or balancing on one leg. I also was performing squats on the balance ball.


What did I do in the group sessions of sport?
When I first arrived, I had to take a test to determine my group level.
The assessment included a 7-minute walking test and also counting how many squats I could do in 30 seconds, among other exercises.
The entire test lasted about 30 minutes. where I was placed in the lower group since I was clearly the weakest performer.
Each session lasted approximately 45 minutes and typically included games such as hangman, archery, and Mölkky.
Regardless of winning or losing, we also performed exercises using resistance bands, dumbbells, and other muscle-strengthening activities.


What was the Anti-Gravity Treadmill like?
You would stand on the machine while it measured your weight.
Then, the outer section would inflate to support the exact percentage of your body weight you selected.
The remaining controls functioned much like a standard treadmill by letting you adjust speed and incline.

Was other Psychological therapy offered?
Yes, they offered a weekly session with a psychologist.
I personally worked with my own psychologist through Google Meet, focusing primarily on CBT and also on mindfulness techniques conducted in English.
Were there any other therapies?
I participated in cooking classes, nutrition workshops, and sessions to discuss physical activities.
What were my specific learnings?
- Balance – I learned the hard way that it’s crucial not to overexert myself on good days, so I can conserve energy and ensure proper recovery.
- Nutrition – I gained a clear understanding of how to consistently obtain the essential nutrients my body needs each day.
Did I have breaks and spare time?
Yes, I had plenty of time to relax each day, since the total daily activity lasted only about two hours.
Did I take my meals together?
Unfortunately, there was no chance to socialise during meals since all food was served in your room.
What happened during Evenings?
The evenings were peaceful and ideal for relaxation, with a curfew set at 9:30 PM every night.
Challenges & Breakthroughs: The Emotional Rollercoaster
What were the hardest parts?
- Chronic Fatigue: Initially, I could only engage in activities for brief periods, but once the fatigue set in, my symptoms—such as drop attacks, difficulty walking straight, and brain fog—would return. The staff were consistently supportive and adapted the sessions to match my abilities.
- Frustration: The first month was incredibly challenging because of chronic fatigue, but this gradually eased as my energy levels improved with consistent daily workouts.
Did I have any breakthrough moments?
I experienced several breakthrough moments during my time there, that allowed me to take control of my FND.
- The importance of regular exercise
- Maintaining proper balance and pacing throughout my activities
- Why good nutrition is essential.
This understanding has empowered me to manage my condition more effectively and improve my overall quality of life.
This felt truly epic and momentous, since now I am able to look ahead and envision the future filled with a strong sense of optimism and genuine hope.

Lessons Learned & Key Takeaways
The power of Neuroplasticity
Our brains are truly amazing but yet truly complex.
Through my rehabilitation journey, I have come to deeply appreciate the brain’s remarkable ability to rewire itself, allowing me to walk again.
The Importance of Consistency & Practice.
I learned that physiotherapy can effectively help improve your FND symptoms.
It is not a magic cure for your symptoms, but a starting point to move toward a better quality of life through continuous effort.
Understanding your Triggers
Through my rehab experience, I have learned that if I overexert myself, my FND symptoms return. Therefore, I value the importance of applying the technique of Balance and Pacing to effectively manage my FND symptoms.
Building a Tool Kit
Beyond balance and pacing, I also learned valuable techniques to manage my FND, including nutrition, exercise, and the crucial role of sleep in recovery.
Self-Compassion
I learned that being kinder to myself means accepting that I will have both good days and bad days. On the bad days, it is essential to relax and avoid feeling guilty.
Post-Rehab: Integration & Continued Journey
What was My transition home like?
As I write this post, I have just returned home after spending eight months between the hospital and a rehabilitation center. My biggest challenge now is readjusting to everyday life while being careful not to push myself too hard.
How will I continue working?
I have devised an exercise plan to continue my rehabilitation at home.
- 3 sessions per week of muscle strengthening exercises using resistance bands
- 2 -3 sessions per week of Nordic Walking
- 2 physio sessions per week
I have also an examination with the movement clinic to see if they will accept me into the day hospital for specialised physiotherapy.
What did I learn about my FND?
I learned that I can improve my symptoms through exercise and effective self-management, including proper nutrition, sleep, and balance.
There is no magic cure for FND, but it is a journey toward a better quality of life.
Relapses may occur, but they are temporary, and you will recover and bounce back!
What is the long-term Impact of Rehab?
Although it is still early, I am very optimistic about the future. To support this, I have planned a 260 km walk over 19 days to raise awareness and funds for FND Hope.

Conclusion
In summary, my time at the rehabilitation center has been truly life-changing. Before I began, I was unable to walk without the help of walking aids, but now I face the future with renewed hope and confidence.
FND massively affects our lives, making it easy to lose hope and doubt the possibility of recovery.
My hope is that by sharing my experience, you will begin to believe that improvement is achievable. In fact, some people can even said recover fully.

- “Are you considering a FND rehabilitation Clinic? Share your questions in the comments below!”
- “Have you been to a rehabilitation Clinic? Share your experience – what was most helpful for you?”
- “If you’re struggling, talk to your doctor about options for going to a FND rehabilitation Clinic.”
Remember. The road to recovery starts with a simple step, that first step is Hope.